Health Equity: Examining How Systemic Racism Has Sickened Our Communities
Siena Ruggeri
April 16, 2019
As the NETWORK community undergoes our Lenten journey through racial justice, we are committed to identifying how racism manifests itself through federal policy. While many are familiar with how racial injustices are perpetuated by our criminal justice system and immigration system, the racism embedded in our healthcare system may not be as evident. Our identity, and especially our racial identity, plays a huge factor in our physical and mental health.
While we must continue to fight for accessible and affordable healthcare for all, that alone will not address the deep racial inequalities in health outcomes. When examining health systems, we must examine how our social location affects our ability to be healthy. Health care cannot be ignorant to identity, because our identity and social location affect both our access to healthcare and our ability to have healthy outcomes.
The healthcare system tends to view people in a vacuum, and often fails to consider how culture, environment, or socioeconomic status affects health. For example, someone reliant on public housing assistance may struggle to get enough exercise when they live in an area that lacks recreational facilities like parks or rec centers. A person with a physical disability might lack the accessible transportation options to get to an appointment with a provider. Type 2 diabetes is difficult to manage living in a food desert with limited access to healthy food options. Many LGBT+ people struggle to find providers accepting of their sexual orientation and may forgo care if there are no safe options in their community. For a non-English speaking patient, a language barrier at the pharmacy can result in inaccurate information on how to safely use a prescription.
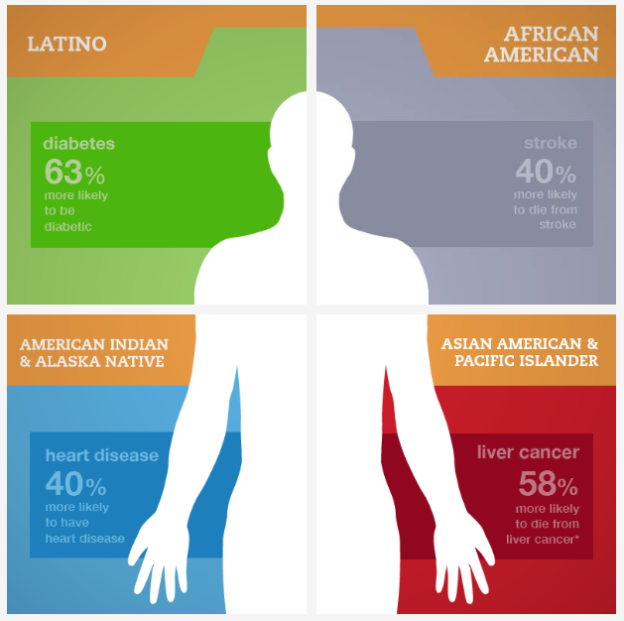
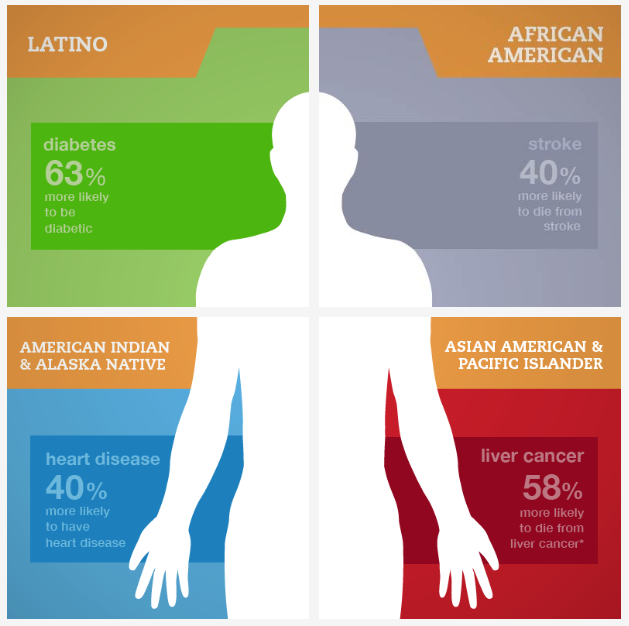
The data is clear– marginalized populations have worse health outcomes. While the exact causes of these outcomes is not completely definitive, it’s clear that these disparities are a result of structural barriers. Black women are four times more likely to die as a result of childbirth than white women. Despite a lower incidence rate of cancer overall, African-American women have a higher cancer death rate when compared to white women. While the opioid crisis is too-often framed as a “white problem,” U.S. opioid death rates for African-Americans have increased over twice as fast as death rates for white individuals.
Like many other inequalities, society often individualizes the problem, blaming specific patients for their failure to “take care of themselves.” We have to break out of this culture of individualism. There are systemic inequalities at play. In fact, there’s a term for it— social determinants of health. The quality and accessibility of health care is only one determinant of health outcomes– other social determinants of health play a massive role. Things like the walkability of our neighborhoods, our access to early childhood education, and how much debt we carry have direct impacts on our overall health. Of course, people of color are disproportionately more likely to have poor social determinants of health. We have a shared responsibility to ensure everyone has the opportunity to be healthy– which means examining our solutions to our broken healthcare system through an equity lens.
We cannot improve health outcomes just by looking narrowly at medical systems. We also cannot continue to approach health in a race-neutral way. The opportunity to be healthy will only be fair and just when we interrogate how systemic inequalities have literally sickened communities of color, and when we redesign those systems to be equitable to all.